Diagnosing the perimenopause
Before we discuss diagnosing the perimenopause it is important to define what is meant by the perimenopause. Having said that, it is very difficult to do so! NICE (National Institute of Clinical Evidence) provide the definition as “vasomotor symptoms and irregular periods”, however it does say that it should be considered if “aged over 45 years with atypical symptoms”. The British Menopause Society defines it as “a change in menstrual cycle pattern when periods become infrequent and the cycles become slightly longer, e.g. 6-7 weeks apart”.
So what symptoms do NICE consider to be “typical”?
Hot flushes/night sweats (vasomotor symptoms)
A sudden feeling of heat in the upper body (face, neck, and chest) that spreads upwards and downwards. In some cases, this becomes generalized, typically lasting 2–4 minutes, and can be associated with excessive sweating, palpitations, or anxiety.
They can be embarrassing and distressing, and triggers may include spicy food and alcohol.
Cognitive impairment and mood disorders
There may be anxiety, mood swings, irritability, sleep disturbance, and reduced quality of life.
There may be low mood (mild depressive symptoms that impair quality of life but are usually intermittent and often associated with hormonal fluctuations in the perimenopause), distinct from depression.
Low mood may be associated with negative beliefs about the menopause, and stigma about age and reproductive status.
There may be poor concentration and memory, and difficulties in multi-tasking, causing social embarrassment.
Urogenital symptoms (genitourinary syndrome of menopause)
These may include vulvovaginal irritation, discomfort, burning, itching, and/or dryness; dyspareunia; reduced libido; dysuria, urinary frequency and urgency, and recurrent lower urinary tract infections.
Symptoms of urogenital atrophy may appear for the first time more than 10 years after the last menstrual period.
Vaginal dryness tends to increase in severity with time since menopause.
Altered sexual function
Vaginal dryness resulting from urogenital atrophy can lead to dyspareunia, which can impact on libido.
Loss of sexual desire and libido may also be a result of declining levels of oestrogen and testosterone as the ovaries fail. The lack of testosterone can be more marked in women who have bilateral oophorectomy.
In addition, low mood, loss of confidence, negative self-beliefs about reproductive status, and altered self-image may contribute to psychological causes for altered sexual function.
Sleep disturbance
This may be due to hot flushes and night sweats disrupting sleep, but may also be due to mood disorders or primary sleep disorders.
Chronically disturbed sleep may lead to fatigue, irritability, and difficulties with short-term memory and concentration.
Other
Joint and muscle pains, headaches, and fatigue are often reported, and may be related to mood disorders or associated with lack of ovarian hormone production.
As we can see from the above definitions there is no consensus of opinion, and certainly no specific blood test cut off value used to make the diagnosis. This means making the diagnosis of perimenopause very challenging, and in any woman over the age of 40 with a range of symptoms it can be considered as a possible diagnosis. There are oestrogen receptors in all areas of the body so symptoms can be varied and more extensive than those listed above. It is therefore important to keep the perimenopause in mind when women develop symptoms in their 40s and 50s. It can of course present even earlier than age 40 for women with premature ovarian insufficiency.
Often the solution is to trial HRT and see if symptoms improve, however even this is not always as straightforward as it seems as there might be issues around the women’s ability to absorb and metabolise HRT affecting its efficacy.
Not all women develop symptoms of the menopause, and women develop symptoms with different hormonal levels so testing is never going to give a definitive answer. It might aid in the diagnosis but should always be interpreted on an individual basis in the context of symptoms.
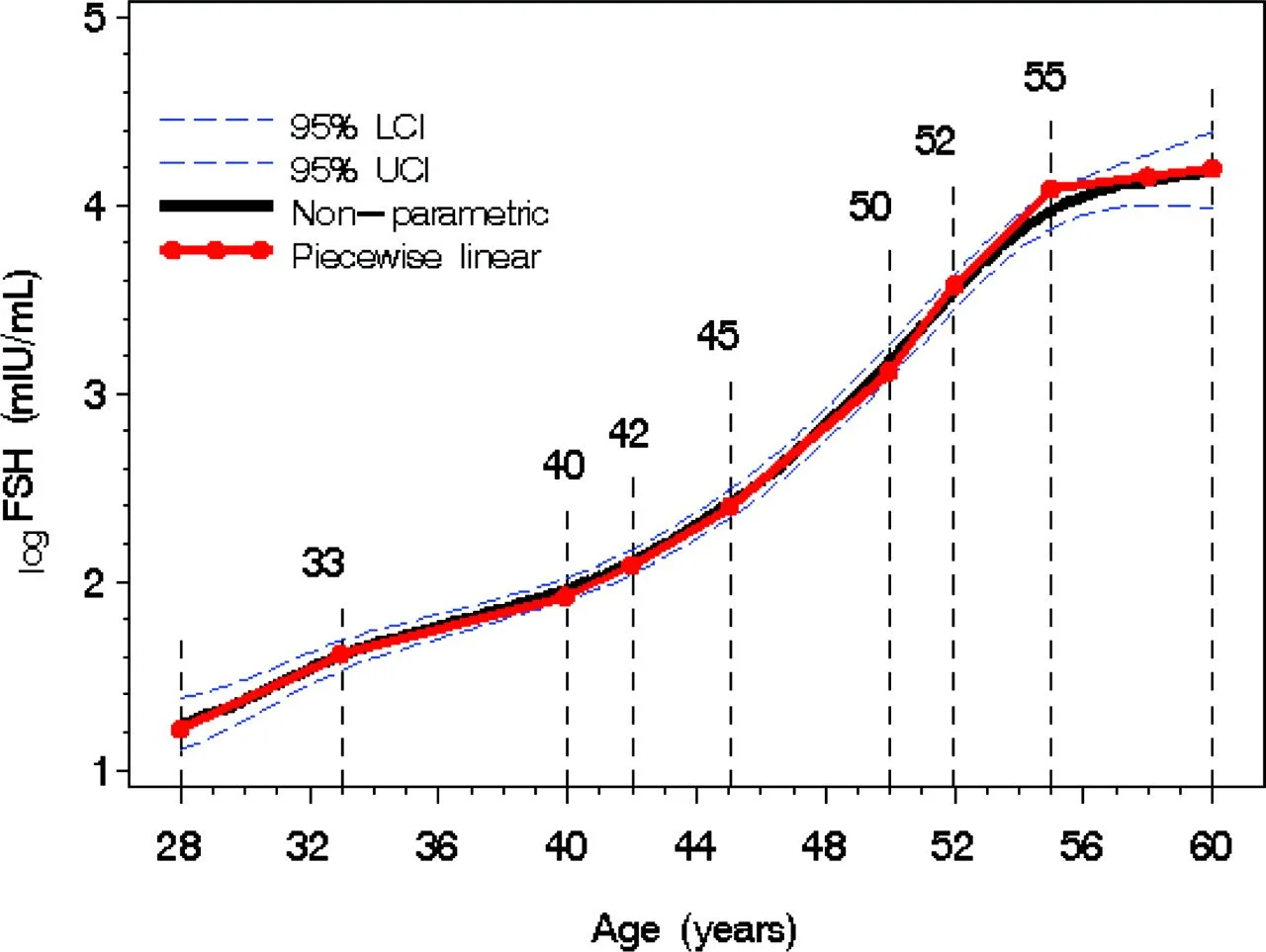
FSH (follicle stimulating hormone) is a test that is done in the NHS for women aged under 45 with classical symptoms or women aged over 45 with atypical symptoms. It is recommend that this is tested twice, 4-6 weeks apart, and a result greater than 3mIU/L (30IU/L) is considered to be a sign of ovarian insufficiency.
As you can see from the chart above FSH levels increase with age and this increase starts to escalate about 7 years prior to the final menstrual period, and then even more rapidly in the 2 years prior to the final menstrual period, however there is variability between individuals as to the rate of change. To detect where on this curve you might be would require serial annual testing, something that can be done privately (about £50/test), or using home urine FSH testing (e.g. Mira home testing kit, £210 for the monitor and £50 for the testing strips). This ideally requires proactive monitoring of FSH levels from at least your early 40s, if not earlier, and before any symptoms occur. If your FSH levels are relatively low and are not showing any rapid rate of change then it is unlikely that your symptoms are being caused by the perimenopause. Conversely if your levels are high, or showing a rapid rate of change then your symptoms might be related to the perimenopause, but this is not definitive. However, some women start to experience perimenopausal symptoms up to 10 years prior to the final menstrual period, and therefore they may not be any detectable changes in the FSH level.
AMH (anti-mullerian hormone) is another hormone that can be used to try to better define how close to the menopause you might be. It is produced by the follicles in the ovary, and therefore as follicle numbers reduce with age the AMH levels also reduce.
The challenge until recently with using AMH levels is that the levels within 2 years of the final menstrual period become so low than they can’t reliably be detected by conventional AMH testing, which is usually done to assist with fertility assessment (costs about £120). A test has been developed in the USA called the MenoCheck which can detect very low levels (measured in picogram/mL rather than ng/ml). Women with AMH levels > 20 pg/mL are unlikely to become postmenopausal in the next 2 years. This can be used as an additional piece of the jigsaw puzzle but as with FSH testing does not necessarily correlate to perimenopausal symptoms. At the moment it is also not offered within the UK so we will have to ‘watch this space’ to see if any laboratories start offering it in the UK.
Full cycle mapping on an at least annual basis may also show signs of the early perimenopause with raising FSH levels, falling oestrogen and progesterone levels, changes in cycle length or more anovulatory cycles over the years (Mira Clarity £270). As ovarian reserve declines, the follicular phase shortens because of decreasing feedback inhibition by follicles recruited during the previous cycle (this is why the first clinical sign of decreasing ovarian reserve is shortening menstrual cycle length.) With the follicular phase starting earlier, estradiol levels start rising closer to menses (and the classic day three FSH peak actually can occur prior to menses). As a result, an elevated day three estradiol level could reflect diminishing ovarian reserve. Cycle mapping can’t be done if any exogenous hormones are being taken like contraception or HRT as it will artificially affect estradiol and progesterone levels, and could be preventing ovulation. Please see my previous blog for more details about cycle mapping https://www.sironahealth.co.uk/blog/cycle-mapping-how-best-to-monitor-your-menstrual-cycle.
References
[1] https://cks.nice.org.uk/topics/menopause/diagnosis/diagnosis-of-menopause-perimenopause/#:~:text=Perimenopause%20%E2%80%94%20if%20the%20woman%20has,is%20not%20using%20hormonal%20contraception).
[2] chrome-extension://efaidnbmnnnibpcajpcglclefindmkaj/https://thebms.org.uk/wp-content/uploads/2023/08/17-BMS-TfC-What-is-the-menopause-AUGUST2023-A.pdf
[3] Sowers MR, Zheng H, McConnell D, et al. Follicle stimulating hormone and its rate of change in defining menopause transition stages. The Journal of Clinical Endocrinology and Metabolism. 2008 Oct;93(10):3958-3964. DOI: 10.1210/jc.2008-0482. PMID: 18647816; PMCID: PMC2579655.
[4] https://shop.miracare.com/en-gb/products/mira-max-ovum-bundle
[5] https://menocheck.com/
[6] Meyers M, Fehring RJ, Schneider M. Case Reports from Women Using a Quantitative Hormone Monitor to Track the Perimenopause Transition. Medicina (Kaunas). 2023 Sep 28;59(10):1743. doi: 10.3390/medicina59101743. PMID: 37893460; PMCID: PMC10608103.